RET (Rearranged During Transfection) is a mutation or abnormal rearrangement of the RET gene that leads to a faulty activation of the cell membrane receptor, basically resulting in the “on-off” switch getting stuck in the “on” position and causing cancer cells to multiply and spread.
RET alterations occur in 2% of non-small cell lung cancers (NSCLC), with a higher percentage of patients being younger (<60) never-smokers. RET alterations also account for 10-20% of papillary thyroid cancers and a majority of advanced sporadic medullary thyroid cancers. Additionally, RET alterations drive an estimated 1-2% of many other cancers, including pancreatic, colorectal, bladder and breast.
Next-generation sequencing (NGS), a method of DNA sequencing, is the only way to detect genetic cancer drivers like RET. NGS can detect RET via tumor tissue or, sometimes, blood (liquid biopsy).
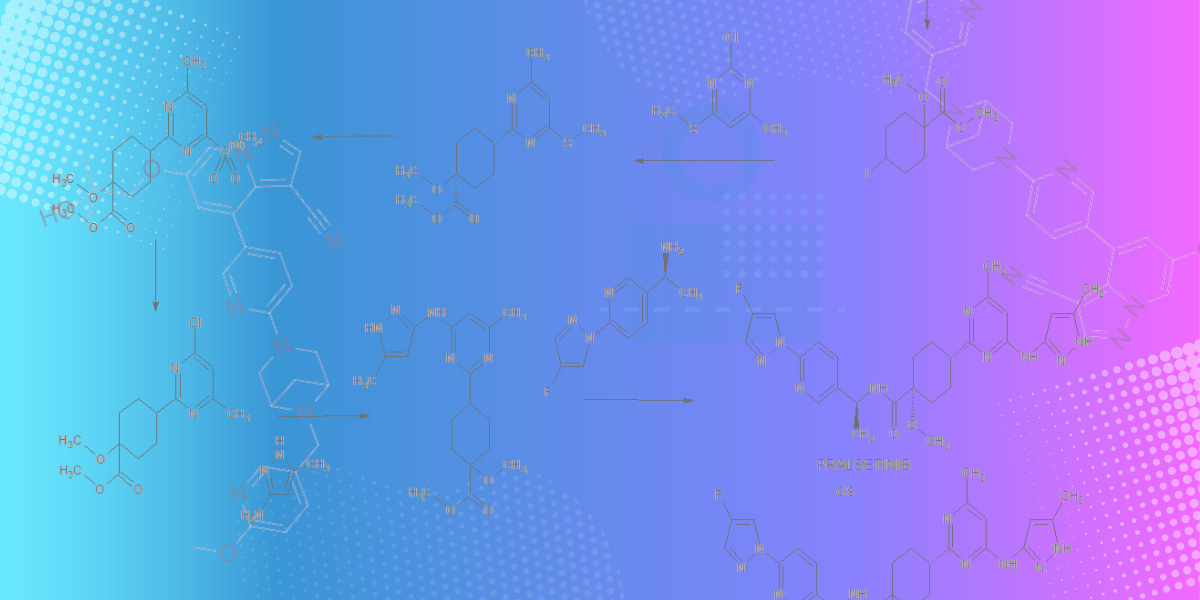
Precision oncology, informed by biomarkers like RET, has evolved rapidly in the last decade, generating more effective targeted therapies with less harsh side effects than previous treatments. In 2020, the FDA approved the first two RET tyrosine kinase inhibitors (TKIs), selpercatinib (Retevmo) and pralsetinib (Gavreto), for RET-driven NSCLC and thyroid cancers. In 2022, the FDA approved Retevmo for treatment of all RET-driven cancers, regardless of tissue of origin (“tissue-agnostic” approval); similar approval is expected for Gavreto in the near future. Both of these highly potent RET inhibitors have shown high central nervous system (CNS) activity, which is critically important as many RET-driven cancers can metastasize to the CNS.
While recent RET-targeted therapies have been pivotal to improving survival and quality of life for RET patients, not all patients respond to these targeted therapies and - for the majority who do - at some point the cancer will progress. There are currently multiple clinical trials assessing RET inhibitors. Other RET patients may experience progression through an off-target or bypass resistance, meaning the cancer finds a new path to grow not dependent on RET; these patients may benefit from combination targeted therapies that target both RET as well as the new alteration/pathway. Additionally, many patients with progression limited to only a few spots (oligoprogression) can often remain on their original targeted therapy while having radiation or surgery to destroy the spots of progression.
After cancer progression on targeted therapies, current treatment options might depend on the cancer tissue of origin (eg lung, thyroid), and/or other relevant biomarkers. Possible strategies might include chemotherapy, radiation, multikinase inhibitors or clinical trials.
RETpositive knows that we must keep driving more treatment options for our community. That's why we support and fund research that will increase the number and quality of cancer treatments for all RET patients.
RET-positive Lung Cancer
-
Abnormal re-arrangement or abnormal fusion of the RET gene occurs in 2% of all lung adenocarcinomas (also called non-small cell lung cancer, or NSCLC). Although this is a small percentage of overall lung cancer cases, given that lung cancer is the number-one cause of cancer-related deaths and that around 1.8 million new lung cancer cases are reported annually worldwide, the number of new RET-positive lung cancer patients diagnosed each year is still considerable - about 20,000-30,000 people yearly.
Overall, NSCLC is more common among women, and RET fusions associated with NSCLC are more prevalent in younger patients who have never or rarely smoked.(3) The most frequent abnormal RET fusion partner genes in NSCLC are RET-KIF5B followed by RET-CCDC6, although at least 30 fusion partner genes have been identified to-date(4). The significance of these fusion variants in terms of overall prognosis remains unclear. -
©LUNGevity Foundation. Used with permission.
Collapsible content
References
1. Kato S, Subbiah V, Marchlik E, Elkin SK, Carter JL, Kurzrock R. RET aberrations in diverse cancers: next-generation sequencing of 4,871 patients. Clin Cancer Res. 2017;23(8):1988-1997. doi:10.1158/1078-0432.CCR-16-1679
2. Li AY, McCusker MG, Russo A, et al. RET fusions in solid tumors. Cancer Treat Rev. 2019;81:101911. doi:10.1016/j.ctrv.2019.101911
3. Subbiah V, Yang D, Velcheti V, Drilon A, Meric-Bernstam F. State-of-the-art strategies for targeting RET-dependent cancers. J Clin Oncol. 2020;38(11):1209-1221. doi:10.1200/JCO.19.02551
4. Mulligan LM. GDNF and the RET receptor in cancer: new insights and therapeutic potential. Front Physiol. 2019;9:1873. doi:10.3389/fphys.2018.01873
RET-positive Thyroid Cancer
Papillary thyroid carcinoma is the most frequent thyroid cancer overall and can be seen with exposure to ionizing radiation. (1) RET rearrangements have been reported in approximately 20% of papillary thyroid cancers, with abnormal fusions between RET and CCDC6 or NCOA4 genes seen most commonly. (2) Although medullary thyroid carcinoma represents 5-10% of all thyroid cancers, activating RET gene abnormalities occur in over 90% of hereditary and approximately 40%-60% of sporadic medullary thyroid carcinoma cases. (3) In contrast to the RET-fusion alterations found in papillary thyroid carcinoma, the RET abnormalities found in medullary thyroid carcinoma are primarily activating point mutations.
The typical age of presentation of sporadic medullary thyroid cancer is in the fifth or sixth decade, and slightly more common in women. In contrast, familial and inherited cases of medullary thyroid cancer often present in those younger than age 20.(4) The identification of RET mutations is relevant to the early diagnosis of hereditary medullary thyroid cancer, and the prognosis of sporadic medullary thyroid cancer.
The role of the RET rearrangements in papillary thyroid cancer is less relevant but still important in patient management, particularly for deciding if or when a targeted therapy should be initiated. (5)
More information about thyroid cancers of all types and a comprehensive list of resources can be found at ThyCa.org.
Collapsible content
References
1. Nikiforov YE, Nikiforova MN. Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol. 2011; 7: 569–580
2. Gautschi Oliver, Rich TA, Reckamp KL et al. Analysis of Cell-Free DNA from 32,989 Advanced Cancers Reveals Novel Co-occuring Activating RET Alterations and Oncogenic Signaling Pathway Aberrations. Clinical Cancer Research Clin Cancer Res October 1 2019 (25) (19) 5832-5842
3. Chu Ying-Hsia, Lloyd Ricardo V. Medullary Thyroid Carcinoma: Recent Advances Including MicroRNA Expression. Endocr Pathol. 2016 Dec;27(4):312-324)
4. Sippel Rebecca S, Chen Herbert, Roy Madhuchhanda. Current Understanding and Management of Medullary Thyroid Cancer. Sept 2013;18(10):1093-1100
5. Romei Cristina, Ciampi Raffaele, Elisei Rossella. A comprehensive overview of the role of the RET proto-oncogene in thyroid carcinoma. Nat Rev Endocrinol. 2016 Apr;12(4):192-202.