RETpositive
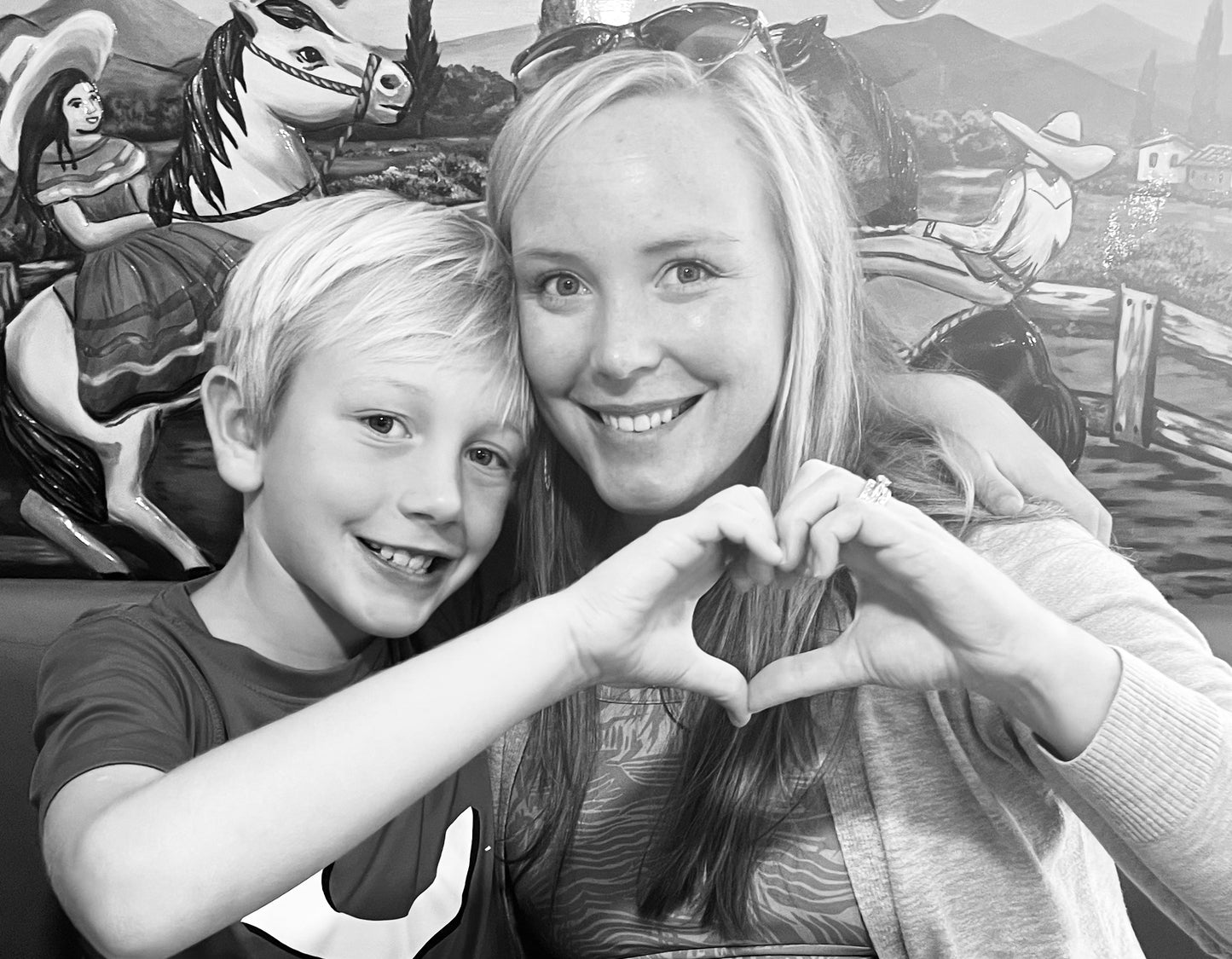
Brittany: 36 at Diagnosis with Stage IV RET+ Lung Cancer
Brittany: 36 at Diagnosis with Stage IV RET+ Lung Cancer
Listen to Brittany share her story. #IAmRETPositive
Brittany was diagnosed with stage IV RET-positive non-small cell lung cancer (NSCLC) at age 36 in 2021.
"In early April 2021, I developed a persistent cough. Being from Kentucky, where seasonal allergies are rampant, and during the height of the COVID-19 pandemic, I decided to err on the side of caution and visit my primary care physician," she says. "We did our due diligence, testing for all the major viruses and treating with steroids, but after six weeks, several new symptoms, and no improvement, I had a chest x-ray. I had developed shortness of breath that was keeping me from being able to stand and sing at church, climb the stairs in my home, and wash my face in the shower. I had also began having ocular migraines.
I had the chest x-ray in June, and within a couple of hours received a call from my PCP. 'Something isn’t right, I’m sending you to pulmonology.' As a healthy 36-year-old with no history of respiratory problems or smoking history, I was only slightly concerned. In mid-July, I met the pulmonologist in his office. He ordered a chest CT to be done the very next day. Within an hour of the test, he called and said, 'I believe you have MAC infection; I’d like to do a bronchoscopy this coming week to confirm.' I had no idea what that meant but a quick Google search had my mind racing. It felt like the worst possible news.
The worst news, however, came just a week later.
Three days after receiving that call, I suffered a stroke. After five days in the hospital, a barrage of tests, and a stumped medical team, the same pulmonologist who had suspected MAC infection came into my hospital room with tears in his eyes to deliver what was the worst possible news – my diagnosis of lung cancer.
The next six weeks were a whirlwind. I endured, as all newly diagnosed cancer patients do, an onslaught of tests, pokes, prods, appointments, and difficult conversations. It was discovered that the shortness of breath and cough were, of course, related to the mass and spread in my lungs. The 'ocular migraines' were mini strokes that had been caused by blood pooling behind my heart and had led to the TIA that stopped me in my tracks. I went on to suffer two more blood clots before finding an anticoagulation regimen that worked.
My oncologist, Dr. Adam Lye at Norton Cancer Institute, has since described my condition as a 'runaway freight train.' The PET scan showed cancer in the lungs, bones and additional lymphatic spread. While he was insistent that I had to have some type of mutation driver because of my age and tobacco naïve status, he was also concerned we were running out of time. The liquid biopsy had not shown any mutations and the bone biopsy from the metastasis in my hip had also come back without news. Determined that the mutation had to be there, Dr. Lye ordered one final biopsy of the primary tumor in the left lung.
In the meantime, I did a combo round of chemotherapy and immunotherapy. Two days after that infusion, I came down with COVID-19 and ended up hospitalized due to severe lung inflammation. My pulmonologist has since said that when I went in the hospital in August, he did not expect me to come out. The cancer, chemo, and COVID combo should have killed me. But my story was not over.
The day before my second scheduled infusion, Dr. Lye called with extreme excitement in his voice. 'We found it! Your biopsy came back with a RET+ KIF5B mutation. This makes up less than 2% of NSCLC patients but there are currently two FDA-approved drugs for your specific cancer mutation. I’m going to start you on pralsetnib (Gavreto) right away. I've been joyfully taking my targeted therapy every day since September 12, 2021. There have continued to be bumps in the road as I adjust to this new normal, but because of research, I was able to celebrate Christmas with my family.
Some day, the cancer will develop resistance to the medicine and the aggressive disease currently lying dormant in my lungs could come roaring back. But I live with the hope that research will continue and there will be advances in my lifetime that can turn the death sentence of RET+ lung cancer into just another chronic condition.



Get Involved
Together we can make RET-positive cancer a chronic disease. Please sign up for our newsletter or make a donation for lifesaving medical research.








